Why Use MRI for Migraine Patients?
Migraines are often diagnosed based on clinical symptoms rather than imaging, but MRI is frequently employed to rule out underlying structural or vascular abnormalities.
Although most MRI scans come back negative in patients with typical migraine symptoms, MRI is crucial for patients with unusual symptoms or those who might be at risk for other neurological conditions.
In particular, MRI can help identify issues like brain tumours, arteriovenous malformations, or strokes, which may present with headache as a symptom.
The ability to rule out these serious conditions provides peace of mind for patients and guides healthcare providers in ensuring the safety of their patients.
Red Flags: When MRI is Essential
Physicians often use MRI to look for “red flags” in headache presentations. Red flags are symptoms or findings that suggest a headache may not be a simple migraine.
These include:
- Onset after age 50: New headaches in older patients may indicate an underlying condition.
- Sudden “thunderclap” headache: A very sudden, severe headache could be a sign of a brain bleed or other vascular issue.
- Focal neurological symptoms: Persistent vision loss, numbness, or weakness may point to a structural brain issue.
- Progressive worsening: A headache that intensifies over time could suggest a condition like a brain tumour.
- Headaches associated with cancer or HIV: These patients are at higher risk for central nervous system infections or metastases.
These symptoms often necessitate further investigation with MRI to rule out serious underlying causes.
MRI Findings in Migraine Patients: What Does the Research Say?
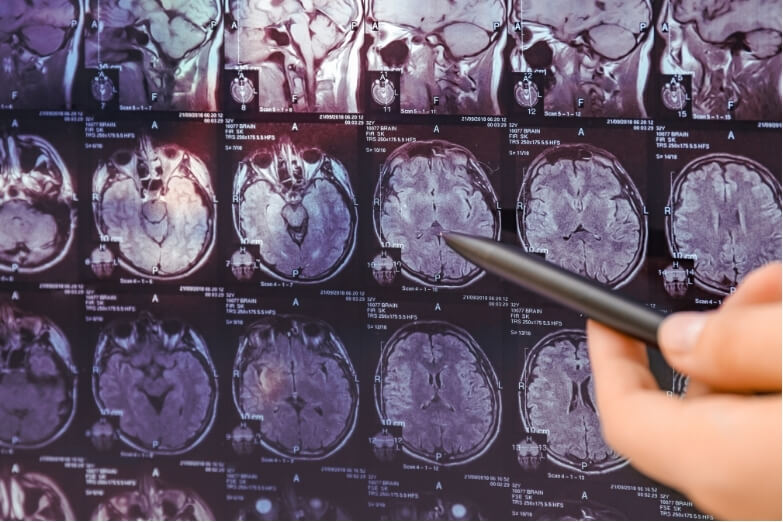
Research has shown that most MRIs for migraine patients do not reveal structural abnormalities, which is reassuring for patients and clinicians.
For instance, a 2022 study found that nearly 90% of patients presenting with migraine had normal MRI scans, supporting the understanding that migraines are often not related to identifiable structural issues in the brain (Freeman, 2022).
However, some studies have noted subtle findings, such as white matter hyperintensities (WMHs), which are small areas of scarring in the brain’s white matter seen on MRI.
Although these are more common in migraine sufferers than in the general population, WMHs are typically benign and not thought to cause symptoms. A study in Cephalalgia noted that these findings, while intriguing, do not appear to impact migraine prognosis or severity in most cases.
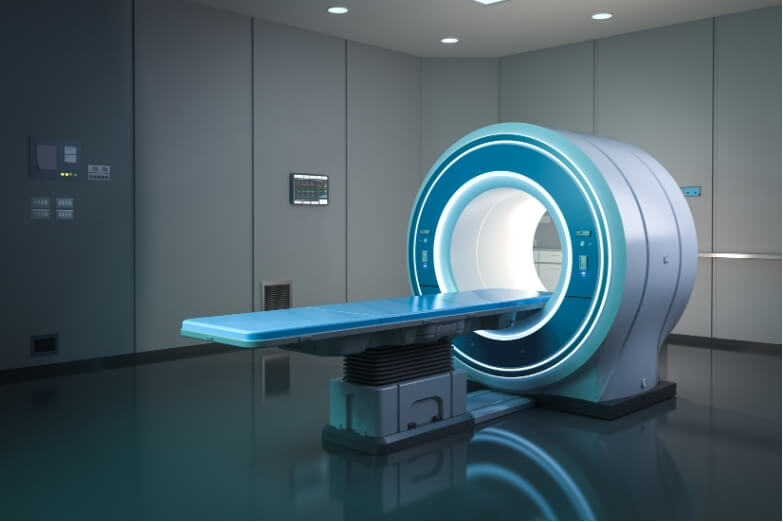
Another emerging area of research is high-resolution or functional MRI, which allows researchers to visualise blood flow and nerve activity.
Studies are ongoing to see if changes in blood flow and brain function during a migraine can help predict attacks or tailor treatments more effectively.
The Future of MRI in Migraine Care
With advancements in MRI technology, there is hope that these scans will eventually allow clinicians to understand more about the brain activity associated with migraines.
Future developments in 7T MRI, which can capture highly detailed brain images, may reveal previously undetectable changes related to migraine activity, particularly in regions involved with pain processing and vascular function (Freeman, 2022).
Researchers are also optimistic about the potential of functional MRI (fMRI) to help identify migraine triggers or patterns, which could be helpful in tailoring treatments. fMRI has already been used in experimental settings to observe changes in blood flow during migraine attacks, giving insights into how migraines affect the brain.
Conclusion: MRI as a Tool for Safety and Insight
While MRIs rarely reveal significant findings in migraine patients, they play an important role in ruling out serious causes of headaches.
For most migraine sufferers, the results are negative, which can reassure both patients and providers that there is no serious underlying issue.
MRI technology continues to evolve, and its role in migraine care may become even more insightful as our understanding of migraine mechanisms grows.